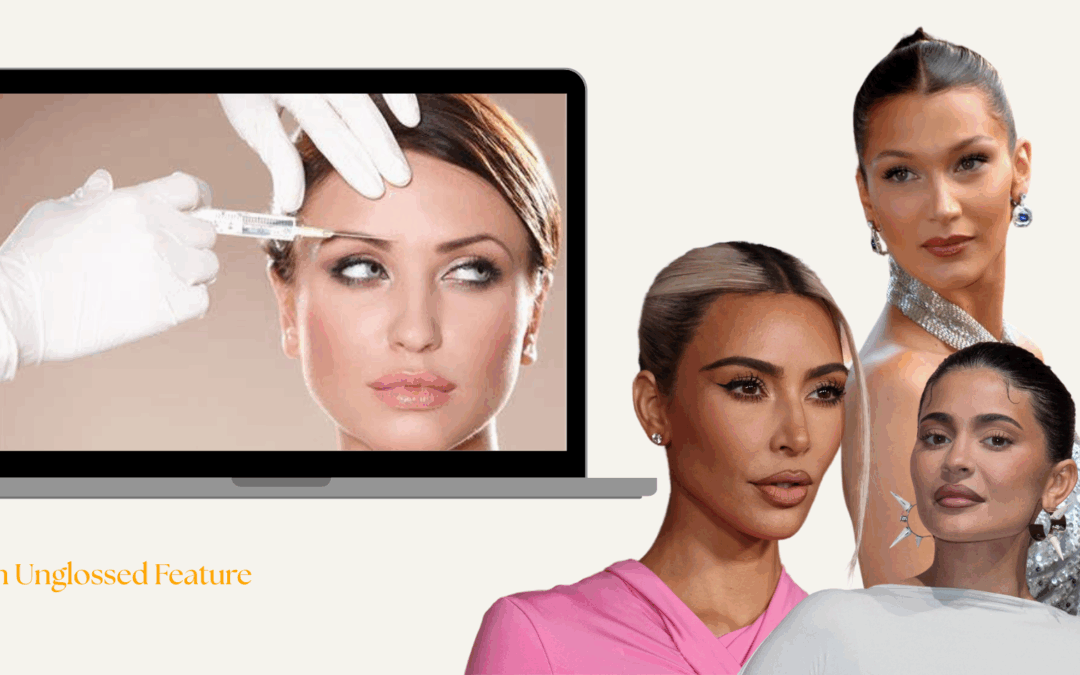
Once a diabetes medication, Ozempic has rapidly transformed into a weight-loss phenomenon, and now, a symbol of privilege. As the drug dominates headlines and vanishes from pharmacy shelves, Tara Nagra investigates what its rise really reveals about class, healthcare, and the cost of chasing thinness.
Once a little-known diabetes medication, Ozempic has rapidly become a household name, and not for managing blood sugar. With global demand skyrocketing by over 300% in the last year, and social media flooded with celebrity endorsements and dramatic weight-loss transformations, Ozempic is no longer just a drug, it’s a status symbol.
Because behind the glossy ‘before and afters’ lies a deeper story about class, access, and the price of health in a system stacked against the less privileged. As a growing number of wealthy users pay hundreds each month for private prescriptions, those the drug was originally designed for, people with type 2 diabetes, are left struggling to access it.
And here’s the cruel irony: the condition Ozempic was created to treat disproportionately affects low-income communities, whilst the medication has become the latest status symbol for the rich. In the UK, people living in deprived areas are nearly twice as likely to develop type 2 diabetes than those in wealthier ones. Yet it’s these same communities who are now struggling to access it.
So while Ozempic is marketed as a ‘fast track’ to thinness, it also reveals a slower, more uncomfortable truth: that health, beauty, and even basic nutrition remain divided by class, where some get to ‘fix’ their bodies, and others are left fighting for the fundamentals.
From behind the scenes of the Ozempic surge, healthcare professional ‘Jane Smith’, whose name has been changed to protect her identity, has seen the impact unfold in real time.
“Over the past 18 months, we have seen a huge surge in the demand for Ozempic, which has caused shortages that predominantly affect our ability to fulfill the needs of type 2 diabetes patients.” she says. “There simply isn’t enough supply to meet the demand, and globally, thousands of diabetes patients have been affected.”
And this shortage isn’t just confined to your local pharmacy. Ozempic’s maker, Novo Nordisk, has faced a global shortage of its active ingredient, semaglutide, since 2022 due to soaring off-label demand for weight loss; an issue that persists into 2025 despite efforts to boost supply.
“The guidelines have had to restrict administering new prescriptions for diabetes patients because there’s just not enough Ozempic to go around, and many patients who were on Ozempic for diabetes treatment have had to stop their medication because the supply is so limited,” Smith continues. “It’s the patients who genuinely need it who are paying the price, because the people managing a serious, long-term illness are being sidelined, while Ozempic is being snapped up for weight loss.”
And much of that snapping up is happening through private healthcare, where patients can pay hundreds per month for fast-tracked access – a price tag that shuts out those dependent on the NHS.
“There’s a noticeable divide between how the private sector and the NHS are handling Ozempic prescriptions,” says Jane. “The NHS is sticking to prescribing Ozempic for type 2 diabetes, but in the private sector, demand is booming, especially in weight loss clinics and online pharmacies. These places are far more flexible, even though Ozempic isn’t officially approved for weight loss.”
She highlights how private patients are willing to pay a premium, and many can get prescriptions with little oversight. “Whether it’s through a private doctor or an online pharmacy, it’s much easier to bypass restrictions, fuelling the shortages even more.” she says.
Talitha Lunnon, a Personal Health Care Assistant, is a clear example of how easily Ozempic can be accessed outside the traditional healthcare system, as she obtained her prescription through an online pharmacy with no waitlists, and no questions. “I started Ozempic last year after hitting a bit of a wall with everything – my weight, my health, my mental state. I tried every diet, every app, every ‘lifestyle change’ under the sun, and nothing seemed to stick. I was just exhausted. So when I heard about Ozempic through social media, I thought maybe this is finally the thing that’ll work.
“To be honest, I didn’t bother with the NHS because I didn’t think I’d qualify, so I turned to private healthcare. It’s £180 a month, which isn’t cheap, but I saw it as an investment in myself. It felt like the only option I had left.”
But Talitha’s story isn’t just about access, it’s about aspiration and privilege. For those who can afford it, Ozempic promises transformation. For those who can’t, it’s just another reminder of what’s out of reach.
Because beyond drugs, the more privileged can also afford personal trainers, organic food shops, and preventive care. Meanwhile, over 9 million adults in the UK live in food-insecure households, where even basic nutrition is a daily struggle. The disparity isn’t just stark, it’s systemic.
Ultimately, Ozempic’s transformation from a life-saving diabetes medication to a luxury weight-loss tool reveals more than just a shift in its use; it perfectly exemplifies the stark inequalities in access to healthcare and nutrition. In a society where thinness is celebrated, healthcare is commodified, and food insecurity is a daily reality for many, Ozempic doesn’t just represent a medical breakthrough, it reflects a system where only the privileged get to ‘fix’ the problems the rest are still forced to live with.
So in the end, maybe Ozempic’s surge isn’t just about who gets thinner, but rather about who gets left behind.